Ankylosing Spondylitis- Symptoms

SYMPTOMS
One of the hallmark features of AS is involvement of the SI (Sacroiliac) joints. This is the joint where the spine and hips join. Episodes of pain and inflammation in this area can make it difficult for the patient to walk or stand. Symptoms often begin in this area and then spread to other parts of the spine. The affected SI joints are usually inflamed unilaterally, and symptoms of pain often will alternate one side at a time.
Pain and stiffness that worsens in the late hours of the night, and upon wakening, are also classic symptoms of AS. The pain can be so severe that the person can barely manage to get out of bed or move in the morning. Typically, once they do manage to get up and moving, the pain and stiffness improve. In fact, this is another factor that can distinguish AS from other types of arthritis. The symptoms seem to improve for most individuals with mild to moderate movement, and they worsen after a night of rest.
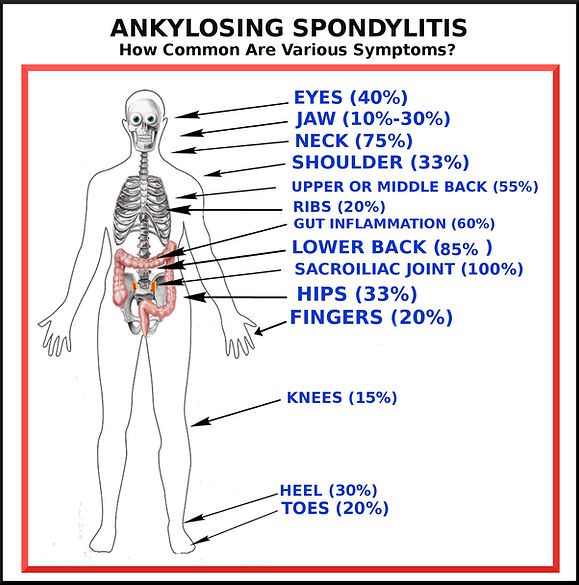
Episodes of pain and inflammation can also be felt in the colon, eyes, jaw, neck, pelvis, heels of the feet, shoulders, fingers, toes, ribs and sternum. The disease does not follow the exact same course among everyone. However, there are some symptoms that tend to be more frequent that others. For example, eye inflammation is considered very common, as well as colon involvement, while cardiac lesions are rare, and shoulder involvement is somewhere in between. In severe cases, the rib cage may become stiffened due to ongoing inflammation, making it a challenge to breath deeply. The overall levels of pain and inflammation can also vary from moderate to severe, depending on the person.
It's important to acknowledge that the inflammation experienced with this disease is systemic in nature. It is not localized only to the bones, ligaments and connective tissues. It affects every part of the body. When a patient experiences a flare up, it is not uncommon for them to feel the levels of inflammation rising throughout their body. This can cause weakness, disorientation, fatigue, and an overall sick feeling. The term "Brain Fog" is sometimes used to describe the feeling of disorientation experienced, as well as difficulty focusing and thinking clearly.
A surprisingly high number of individuals with AS also experience Inflammatory Bowel Diseases, such as Crohns Disease. A number of patients with AS also have some skin manifestations such as Psoriasis, at one time or another.
Another common symptom of Ankylosing Spondylitis is Enthesitis (inflammation of the entheses, which is the area where joints, tendons or ligaments attach to bones). This causes pain, swelling and tenderness in multiple sites around the body...the heel of the foot, chest, sacroiliac joints, in between vertebrae of the back and neck, and pelvis.
It is the Enthesitis that leads to fusion of the vertebrae over time. This happens after repeated episodes of inflammation of the entheses. The body acts to heal and repair the area that was damaged by inflammation. It does this by attempting to reinforce the apparently vulnerable area by depositing calcium there, which leads to extra bone formation that eventually bridges the vertebrae together. After repeated episodes, the spine eventually becomes one long, solid bone. If this happens, the person has a higher risk of fracture because the new bone formed is inherently weaker than normal bone, and the fusion results in a restricted range of movement. However, not everyone will experience fusion, especially if they take serious steps to manage their disease.
One cannot talk about the symptoms
of Ankylosing Spondylitis without
mentioning the sometimes debilitating
fatigue that is associated with the
illness. In fact, next to pain, fatigue
is the next biggest complaint among
those who suffer from AS.
This level of exhaustion is not the same
as just feeling tired. It is a result of the
inflammation process itself, combined
with sleep disturbances that are
common with AS. These sleep
disturbances can be due to physical
pain and discomfort, which typically
worsen at night.
But how does the inflammatory process
cause fatigue? During periods of inflam-
mation, cytokines are released. This
can cause feelings of exhaustion. Your
body is expelling energy to counteract
the inflammation. In addition to this,
inflammation can cause anemia. It is
called "Anemia of Chronic Diseases" or
"Anemia of Inflammation". With this
type of anemia, red blood cells are not
functioning normally and cannot absorb iron efficiently. At the same time, the body is not responding normally to EPO (erythropoietin). This is a hormone that the kidneys produce in order to stimulate bone marrow production of red blood cells. Over time this leads to a lower than normal amount of red blood cells. The resulting anemia adds to the exhaustion.
So the combination of your body fighting inflammation, sleep disturbances from pain and discomfort, and a possible underlying anemic condition, all contribute to the exhaustion and fatigue that is so commonly associated with Ankylosing Spondylitis. By reducing inflammation (preferably while avoiding NSAIDs), you will reduce the pain, sleep better, and address the underlying cause of anemia (if present).
OTHER POSSIBLE SYMPTOMS OF ANKYLOSING SPONDYLITIS:
1. Neurological Complications- Due to pressure on the lower portion of the spinal chord (called cauda equina), the inability to control bladder and bowel functions may develop, as well as a loss of reflexes in the ankles.
2. Cardiac Complications- There are a number of cardiovascular diseases and conditions which have been linked to AS. Some of these develop or exist even before AS is diagnosed. These conditions can include inflammation of the aorta (Aortitis). The Aorta is the large artery that carries blood from the heart to the entire body. When inflammed, the Aorta may not be able to provide enough blood to the rest of the body and high
blood pressure may result. In addition, ongoing inflammation may result in the Aortic valve becoming "leaky" and regurgitating, allowing blood to flow backwards. This can result in dizziness, chest pain, and shortness of breath. Surgery may be required to repair the valve. Aortic incompetence has been noted in 3.5% of AS patients who have had the disease for 15 years, and in 10% of those who have had the disease for 30 years.
Arrhythmia has also been linked to some cases of Ankylosing Spondylitis, resulting in the heart either beating too fast, too slow, or skipping beats. The resulting symptoms are usually chest pain, shortness of breath, a feeling of lightheadedness, dizziness and fatigue. These types of disturbances in the heart beat can, in extreme cases, even result in cardiac arrest. They are usually treated with either the installation of a pacemaker, or medication, defibrillation, or a combination of these. Cardiac conduction disturbance (arrhythmia) has been noted in 2.7% of AS patients who had the disease for 15 years, and 8.5% after 30 years. This clearly shows that it is the ongoing inflammation that causes increased damage over time to the heart and its components. Therefore, earlier diagnosis, and better management of inflammation can apparently reduce the likelihood of these relatively rare complications.
Cardiomyopathy is another cardiac complication that can be linked to Ankylosing Spondylitis. At first the connection was only suspected, but now further studies and research have proven it to be a clinical reality. For example, in one particular echocardiographic study of patients with AS, evidence of cardiomyopathy was found in 32.2% of adult-onset individuals. (1)
How does the prevalence of cardiomyopathy among Ankylosing Spondylitis patients compare to the prevalence of this disorder among the general population? Well, among those with Ankylosing Spondylitis, every 400-800 individuals among 100,000 are estimated to have dilated cardiomyopathy, whereas among the general population, only 8.3 - 36.5 people among 100,000 are estimated to have this condition.(1) Therefore, we see a significant increase in risk among those with AS, and the estimate of those with AS who have cardiomyopathy might actually be underestimated because symptoms in the early stages are often not detectable. Also, doctors do not always connect the dots and relate the cardiac condition of their patients to their autoimmune arthritic condition. Decreased exercise intolerance may be attributed to Ankylosing Spondylitis itself, and not to an underlying heart problem that is related to AS. Cardiomyopathy is usually detected only once it has become advanced. Since AS often presents itself in relatively young individuals, a heart disorder is not the first thing suspected when symptoms present.
What exactly is Cardiomyopathy? This is a disorder with impaired ventricular function that enlarges and weakens the heart muscle, making it more difficult for the heart to adequately supply blood to the rest of the body. Left untreated, it can result in valve problems, blood clots, heart failure, and even cardiac arrest. The symptoms include shortness of breath (not only during exertion), swelling of ankles, legs and feet, fatigue, abdominal bloating, and an irregular heartbeat. It is typically controlled by managing the symptoms involved, taking steps to prevent the condition from worsening, and therefore reducing risks for additional complications. Blood pressure medications might be administered to help improve the heart's ability to pump, and beta blockers might also be used to aid in improving heart function. A pacemaker might even be recommended, to better coordinate the contractions between the ventricles.
There have been cases noted where better control of the underlying inflammatory process related to Ankylosing Spondylitis led to partial improvement of the ventricular function of the heart, and therefore, improvement in the Cardiomyopathy. (1)
Another heart disorder related to Ankylosing Spondylitis includes Ischemic heart disease, or Atherosclerosis. This is characterized by a reduced supply of blood to the muscle of the heart, typically due to coronary artery disease. Symptoms include chest pain and pressure, decreased tolerance for exercise, shortness of breath, etc. Medications used to lower blood pressure and cholesterol may be given, as well as nitroglycerin. In more severe cases, bypass surgery may be needed, or angioplasty.
Myocardial infarction (otherwise known as a heart attack) is believed to be 3-4 times greater in prevalence among the AS population than the general population (1.2).
Overall, a study done in 2011 by Canadian researches discovered that having Ankylosing Spondylitis increases your risks for heart disease AND stroke by 25-60% (2). Why the big range? This is because each type of heart disease or stroke has a different risk factor. For example, there was a 60% higher risk for valvular heart disease, between a 30%-40% higher risk for ischemic heart disease, and a 25% higher risk for ANY cardiovascular disease diagnoses. They also had a 30% higher risk for being hospitalized for a cardiovascular disease compared to the general population.
So why does having AS increase risk for heart disease of various types, and strokes? The answer is not fully known, but the correlation between the risk and the ongoing chronic inflammation has been associated. Also, the use of NSAIDs increases the risk of heart complications, and perhaps also the fact that patients with AS typically are not able to be as active and exercise as much as the general population, primarily due to pain and fatigue.
What can you do to reduce your risks? Well the most obvious thing you can do is to quite smoking immediately if you have that habit. In addition to that, keep the inflammation under control as much as possible. This website provides information on how diet can drastically reduce your inflammation and associated pain. Also, avoid NSAIDs. Not only do they damage your gut, and therefore keep provoking the cycle of disease, but they also are shown to significantly increase your risk of cardiovascular events. In fact, one study in 2011 showed that those who use NSAIDs on a long-term basis have a 2 - 4 time increased risk for a stroke, heart attack, or cardiovascular-related death. Once your inflammation is better controlled, your fatigue will also lessen significantly. Then you will be in a great position to increase your levels of activity and exercise.
3. Costochondritis - This condition feels very similar to a heart attack, but actually does not involve the heart at all. Although painful, it is a harmless inflammation of the cartilage that connects the ribs and the sternum. The pain, indeed, can be excruciating. Typically it will subside on its own, but in some cases it might last for a few months. It can be relieved, however, with pain medications, antidepressants and even the epilepsy drug Gabapentin. Injections of numbing medications can also help.
4. Lungs- There are a number of pulmonary manifestations of Ankylosing Spondylitis. These include: apical fibrobullous disease (scarring or fibrosis develops, especially at the top of the lungs), interstitial lung disease, secondary infections (Aspergillus fumigatus, a fungus, is the most common pathogen), chest wall restriction, obstructive sleep apnea, bronchiectasis and spontaneous pneumothorax.
When fibrobullous lesions develop, many of the lesions are progressive and coexist with nodules, as well as the formation of cysts and cavities. So far, no pharmaceutical treatments are known to alter the course of apical fibrobullous disease once it develops, including anti-inflamatories and immune suppressants.
Bronchiectasis results from fibrosis pulling the airways apart, making them wider, damaging the walls of the bronchial tubes. However, damage to the walls can also be caused by frequent infections, whether fungal or mycobacterial. It is unknown if the increased frequency of bronchial (airway) damage associated with AS is more attributed to the disease process causing fibrosis, or if it is caused by the immune suppressant drugs commonly prescribed to AS patients, making them more susceptible to infections. (2.5, 2.8)
Also, restricted chest wall movement due to stiff ribs may decrease the ability of of the lungs to expand. Breathing, therefore, can become a challenge. What can you do? Smoking absolutely must be ceased! Also, take steps to manage the underlying inflammation (not with NSAIDs), and try deep breathing exercises and stretches that help to keep the chest wall more limber.
5. Kidney Stones- It has been suggested that patients with AS have an increased risk for developing kidney stones than the general public, based on the findings of researches in Taiwan (3). In this population based study, newly diagnosed cases of kidney stones were found to be 19% more common among patients with Ankylosing Spondylitis, compared to those in the population who do not have this type of arthritis. Kidney stones are primarily made of calcium, and it has been demonstrated that an altered metabolism of vitamin D and calcium can be found among those with AS. This is suspected to be one of the factors involved. Also, if anti inflammatory drugs are prescribed to a patient for AS, this increases the risk of kidney stone formation (nephrolithiasis). Thus we have yet another reason to avoid NSAIDs.
6. Spinal Fractures- Patients with Ankylosing Spondylitis are highly susceptible to unstable spinal fractures, and associated neurological damage, with the most minimal trauma, including low impact activities, falls, accidents, or incidents. In fact, fractures of the spine are four times more common and spinal cord injuries are 11 times more common (4) among the AS population. The increased susceptibility to fractures, even from just a trivial injury, is due to a variety of factors.
During the disease process, the spinal ligaments tend to undergo ossification. Also, as a response to frequent periods of inflammation, additional bone tends to be created that bridges the vertebrae together. This new bone is always more fragile and weak than normal bone. As the bridges between the vertebrae connect, the spine becomes immobile as one, long fixed bone. This, combined with the ossified ligaments, leads to immobility of the spine. It looses flexibility. Upon impact, it is normally the flexibility of the vertebrae and the cushions between them (discs) that typically absorb impact in a healthy spine. Think of a spring compressing and expanding when under pressure. Without this function, the spine simply fractures instead of compressing or moving when impact or jarring occurs. The ability to absorb even minor impacts is lost.
Another factor that contributes to the increased risk for spinal fractures is that AS patients often have an altered gait due to pain, inflammation, or partial fusing. This altered gait can impair their balance and place them at a greater risk for falls. If they have kyphosis, then the compromised ability to see in front of them, due to spinal deformity, also increases the risk for falls.
Ways To Limit The Risk For Fractures:
1. Avoid drinking alcohol. Anything that can alter your balance or gait puts you at a higher risk for falls.
2. Avoid narcotics or opoids for the same reasons listed above. For a Non-Drug approach to managing pain, check out the rest of this website.
3. Make modifications to your home. Install grab bars in the tub or shower. Remove throw rugs, which are a trip hazard. Improve lighting and use night lights. Keep pathways free of anything that could be tripped over: clutter, loose chords, shoes in the floor, plants, boxes, magazine racks, etc. Use a non-slip mat in the tub or shower. Repair loose floorboards or wobbly tiles.
4. Use shoes without laces, make sure they are the proper size, and only wear shoes with low heels.
5. Avoid contact sports, also referred to as collision sports (boxing, martial arts, rugby, football, hockey, soccer, wrestling, basketball, diving, lacrosse, rodeos, skiing, handball). Even limited contact sports can pose a danger (baseball, cheerleading, softball, volleyball, gymnastics, etc). And high-impact sports which do not involve collision, still put stress on your spine and can increase your risk for fractures (horseback riding, running and jogging, for example). Depending on whether or not you have been cleared by a doctor as having NO fusion, you will adjust your choices of sports and exercise accordingly. How far your disease has progressed will alter some of your choices, although contact and high-impact sports are never recommended. You might decide to engage in some sports that do not NORMALLY involve collision or impact, but still have a risk for possible injury (such as bicycling) if you fall or crash. You might also find that you need to avoid sports that require twisting (golf, tennis).
One of the best sports for a patient with Ankylosing Spondylitis is swimming (completely non impact as long as you avoid diving). The breaststroke can help maintain chest expansion, and overall swimming helps to increase the flexibility in your spine without jarring it. Some patients with AS also enjoy rowing, fishing, speed walking, ballroom dancing, yoga, Pilates, Tai Chi, aerobics, badminton, etc. And of course there are sports which do not involve much or any physical activity but still add to the enjoyment of life (chess, sailing, darts, poker, star gazing, etc). In addition to sports, there are exercises and stretches which are very beneficial for all AS patients to engage in. Some of these are outlined on this website.
6. When riding in a car, always use your seat belt. Drive defensively and leave plenty of room between yourself and the car in front of you. Observe speed limitations. If your ability to turn your neck and check your blind spots is limited, then purchase a "No Blind Spot Rear View Mirror". This is the same type of mirror used by police officers and professional race car drivers. Some of them just snap over your existing rear view mirror and do not require any special installation. They completely eliminate your blind spots. You might also choose to purchase a vehicle with a built in rear view camera (for backing up), or you can buy an after-market rear view camera to add to your vehicle if it did not come with one already.
7. Have your eyes checked at least once a year by an Eye Doctor. If you need corrective lenses, use them!
8. Avoid stairs. If necessary, always hold onto the railings. There should be railings on both sides.
9. If any of your medications are making you tired, groggy, dizzy or disoriented, review them with your Doctor and consider different options.
10. Keep clothing, dishes, food and other necessities that you frequently need, in an easy to reach location so that you are not tempted to climb on a stool or ladder.
11. Do not climb on a stool or ladder!
Most fractures with Ankylosing Spondylitis occur in the neck. It's also important to note that the majority of these fractures are not detectable by radiographs (x rays). An MRI or a CT image are more sensitive and should be used when a possible fracture is being investigated. In fact, any time a person with AS experiences a fall or injury, it is good to employ one of these imaging techniques just to make sure there are no hidden fractures. It is important to discover these fractures so that you can receive proper bracing to stabilize the area and avoid further serious injuries, either to the spine, the spinal cord, or both.
Sources:
1. Cardiomyopathy in Ankylosing Spondylitis, NAI LEE LUI, JULIAN THUMBOO, AND ROBERT INMAN, Arthritis Care & Research Vol. 63, No. 4, April 2011, pp 564 –569, DOI 10.1002/acr.20333
1.2 Ankylosing Spondylitis: A Risk Factor For Myocardial Infarction? Peters MJ, Visman I, Nielen MM, Van Dillen N, Verheij RA, van der Horst-Bruinsma IE, Dijkmans BA, Nurmohamed MT, Ann Rheum Dis. 2010 Mar;69(3):579-81. doi: 10.1136/ard.2009.110593. Epub 2009 Apr 28.
2. Increased Risk of Cardiovascular and Cerebrovascular Diseases in Individuals With Ankylosing Spondylitis, Shelagh M. Szabo, Adrian R. Levy, Sumati R. Rao, Stephanie E. Kirbach, Diane Lacaille, Mary Cifaldi, and Walter P. Maksymowych, ARTHRITIS & RHEUMATISM Vol. 63, No. 11, November 2011, pp 3294–3304 DOI 10.1002/art.30581
2.5 Pulmonary Manifestations of Ankylosing Spondylitis. Kanathur, Lee-Chiong T. Clin Chest Med. 2010 Sep;31(3):547-54. doi: 10.1016/j.ccm.2010.05.002.
2.8 Bronchiectasis and Autoimmune Disease. / Dhasmana, Devesh Janardan; Wilson, Robert. European Respiratory Monograph: Bronchiectasis. ed. / RA Floto; CS Haworth. Vol. 52 European Respiratory Society, 2011. p. 192 DOI: 10.1183/1025448x.10004310 (Bronchiectasis). Research output: Chapter 13 in Book/Page 10/Report/Conference proceeding › Chapter (peer-reviewed)
3. The Risk of Nephrolithiasis Among Patients With Ankylosing Spondylitis: a Population-Based Cohort Study, Mu Tsun SHIH, Shou Hung TANG, Tai Lung CHA, Sheng Tang WU, Jen Huai CHIANG and Wen Chi CHEN, Archives of Rheumatology Vol. 31 Issue 4, December 2016, pages 346-352, DOI: 10.5606/ArchRheumatol.2016.5938
4. Management of Acute Spinal Fractures in Ankylosing Spondylitis, Saad B. Chaudhary, Heidi Hullinger, and Michael J. Vives, ISRN Rheumatol. 2011; 2011: 150484 DOI: 10.5402/2011/150484